What is MEN3 (formerly MEN2b)?
MEN3, also known as MEN2B (Multiple Endocrine Neoplasia type 2B), is a rare genetic disorder involving the development of tumors in specific endocrine glands. There are two main tumors common to MEN3. These occur in the butterfly-shaped thyroid gland in the neck, and less commonly in the adrenal glands that sit on top of each kidney. The tumor in the thyroid gland is always cancerous (medullary thyroid cancer or MTC) and is more aggressive in MEN3 than in those of MEN2. Each type of tumor may occur alone and independently of MEN.
Blood and urine tests for hormone levels as well as scans of the neck and abdominal area are all used to check for tumors. If a tumor is found surgery may be needed to remove either just the tumor itself or the whole of the affected gland. This is necessary as early as possible in childhood for the medullary thyroid cancer.
-
MEN2B and Me: Ethan's Own Words
How is the RET gene involved in MEN3?
Like MEN2, MEN3 is caused by specific mutations in the RET gene, which plays a key role in cell growth and signaling. These mutations lead to uncontrolled cell division and the development of tumors in endocrine glands. Also similar to MEN2, only one parent has to carry the genetic mutation in order to have a 50% chance that the child will inherit it as well.
Symptoms of MEN3
The most notable feature of MEN3 is medullary thyroid cancer (MTC), which can also develop in MEN2, but it tends to be more aggressive and appears at an earlier age in MEN3 patients. Many individuals also develop high blood pressure, heart palpitations, and excessive sweating. MEN3 is also uniquely associated with mucosal neuromas (small, benign growths on the lips and tongue). Sometimes, individuals with MEN3 may have a tall, slender body build with long fingers and limbs (called a marfanoid habitus), but this is not always present. Let’s look at how MEN3 affects different parts of the body.
Medullary Thyroid Cancer and MEN3
Almost 10 out of 10 (100%) of MEN3 patients will develop medullary thyroid cancer (MTC) sometimes within the first year of life. The thyroid is the butterfly-shaped gland found at the base of the throat in the front of the neck. Thyroid cancer or pre-cancerous hyperplasia may be found using blood tests to measure levels of calcitonin. Treatment involves an operation to remove the thyroid gland and the nearby lymph nodes (total thyroidectomy and central lymph node dissection).
After surgery lifelong medicine called levothyroxine needs to be taken. If calcitonin is detected after the operation, further surgery and other therapies are used to control it. MTC is usually slow growing and may often be managed effectively in this way without symptoms for many years. Children identified as having MEN3 are offered a thyroidectomy within the first year of life. Parathyroid glands are sometimes unavoidably removed at the same time as the thyroid gland (see below).
-
 Diagram of the Parathyroid Glands
Diagram of the Parathyroid Glands
MEN3 and the Parathyroid Glands
These small glands lie just next to or are sometimes embedded within the butterfly-shaped thyroid gland in the neck and help to control calcium levels in the body. Owing to their location, these glands may be unavoidably removed or injured during thyroid surgery. If the parathyroid glands are removed or injured, patients will usually have to take a daily Vitamin D capsule to help the body absorb calcium from the diet.
Adrenal Glands and Phaeochromocytomas
The body’s two adrenal glands are normally each about the size of a whole walnut and sit just on top of the kidneys. A tumor of the inner part of the adrenal gland is called a phaeochromocytoma (fee-o-cromo-sy-toma) and is almost always benign (not cancerous) in MEN. Phaeochromocytomas may grow for many years without causing severe symptoms but can be activated by events such as childbirth or surgery. Symptoms are varied and may include all or some of the following: sudden migraine-like headaches, palpitations, breathlessness, excessive sweating, high (or rarely low) blood pressure (constant or off- and-on), trembling, tiredness, depression, anxiety, and nausea with or without vomiting.
These tumors may be detected using blood and urine tests as well as several different types of scan. Treatment involves an operation to remove the gland and tumor. A period of medicine before surgery is necessary to control the unstable blood pressure. If both adrenal glands are removed, lifelong steroid replacement therapy is necessary.
-
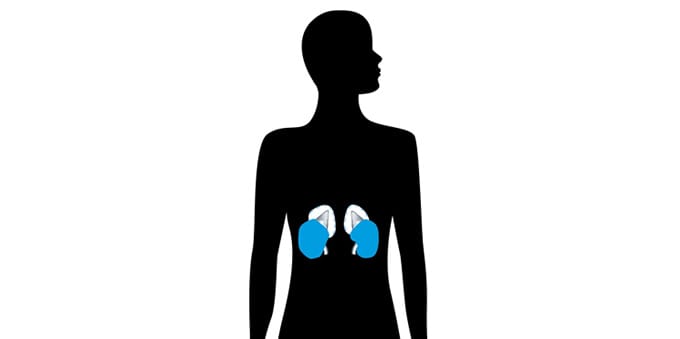 Diagram of the Adrenal Glands
Diagram of the Adrenal Glands
When Should Someone Be Screened for MEN3?
Screening for MEN3 is recommended for individuals with a family history of the condition or those with signs such as marfanoid habitus or mucosal neuromas. MEN3 is an inherited condition that only requires one parent to pass on, and having one parent with MEN3 gives you a 50% chance of having it as well. Much like with the other MEN syndromes, early screening is essential to managing symptoms, particularly the development of thyroid cancer.
What Is the Life Expectancy for Someone With MEN3?
With early diagnosis and proper management, MEN3 does not have to be life-threatening. However, medullary thyroid cancer (MTC) associated with MEN3 is more aggressive and develops earlier than in other MEN syndromes, so early screening and preventive thyroidectomy are crucial for improving long-term outcomes.
Pheochromocytomas, another common feature of MEN3, can cause high blood pressure and other cardiovascular issues if not treated, but early detection and surgical removal can reduce associated risks. Regular screening and medical monitoring for other tumors and complications are key to ensuring the best quality of life.
Author: Jo Grey, AMEND CEO, with the help of the AMEND Medical Advisory Team. Updated by John Metzcar
Further Reading
-
MEN3 Patient Information Book (UK)

Updated 3rd edition of this popular book on MEN2B (aka MEN3) by AMEND in the UK.
View Booklet
VIDEOS
The following films were produced by AMEND UK in early 2019 to raise awareness of MEN2B, to encourage earlier diagnosis, and to support other patients.
Hard of hearing? These films are available with subtitles via their YouTube channel.
Funded by AMEND and a grant from The Society for Endocrinology.
-
MEN2B and Me: Asher (Diagnosed at 6 weeks)
-
MEN2B and Me: Ethan (Diagnosed at age 12)
-
MEN2B and Me: Kristina (Diagnosed at age 2)
Patient Stories
Click here to read patient stories about MEN2B
-
My Story Template
Want to write your own story but don't know where to start? Use our handy template for inspiration! Just scan and send by email or pop it in the post.
Click here to download the template