What is MEN1?
MEN1 syndrome (Multiple Endocrine Neoplasia type 1) is a rare genetic condition affecting about 1 in 30,000 people. It can cause tumors to develop in certain glands in the body. There are three main types of tumor that can occur in MEN1, and they are usually not malignant or cancer (benign). They occur in the parathyroid glands in the neck, the endocrine pancreas and gut (duodenum) and the pituitary gland under the base of the brain behind the nose.
80% (8 out of 10) of MEN1 patients will have developed at least one of the tumors by the age of 50, and 43% (4 out of 10) by the age of 20. Younger cases have been recorded. The condition varies greatly even within families; not everyone will have the same tumors and they will not occur at the same age. Not all MEN1 patients will have all of the tumors described here.
Blood tests to look at hormone levels and scans of the head, neck and abdominal area are all used to check for tumors. If a tumor is found, surgery may be needed to remove either just the tumor itself or the whole of the affected gland. In some cases treatment with controlling medicines may be used.
-
MEN1 Patient Experience
What is the MEN1 gene?
The MEN1 gene plays a crucial role in the body by providing instructions for the creation of a protein called menin, which helps regulate cell growth and prevent tumors. Mutations in the MEN1 gene lead to Multiple Endocrine Neoplasia type 1. Families with a history of MEN1 should be aware that children only need one altered copy of the gene to develop the condition, which means that only one parent needs to have MEN1 to be at risk for the disorder. Luckily, genetic testing in early childhood can help MEN1 patients live long, normal lives.
MEN1 Symptoms
Since MEN1 primarily affects the parathyroid glands, pancreas, and pituitary gland, the symptoms are often related to the overproduction of hormones by these organs. The most common manifestation of MEN1 is overactivity of the parathyroid glands (hyperparathyroidism), which occurs in nearly all MEN1 patients. This leads to high levels of calcium in the blood (hypercalcemia), which can cause a variety of symptoms. Let’s look at how each area of the body is impacted by MEN1:
Hyperparathyroidism in MEN1
Parathyroid glands lie just next to or are sometimes embedded within the butterfly-shaped thyroid gland in the neck. More than 9 out of 10 (90%) of MEN1 patients will develop a parathyroid tumor called an adenoma. These tumors release large amounts of parathyroid hormone (PTH) and so can be easily found using blood and urine tests.
Some symptoms of an untreated parathyroid tumors include irritability, ulcers, kidney stones, pancreatitis, bone fractures, osteoporosis, tiredness, muscle or bone pain, indigestion, poor memory and constipation. However most patients will have very few of these symptoms particularly when diagnosed and treated early on. At the moment, the recommended treatment for parathyroid tumors is a relatively small operation to often removing almost all four glands and involves only a few days in hospital. Medicines are available to control parathyroid growth where surgery is not possible. After parathyroid glands are removed, patients may have to take a Vitamin D capsule to help the body absorb calcium.
Patients who have parathyroid gland tumors may develop:
- Fatigue and weakness
- Bone pain or osteoporosis
- Kidney stones
- Abdominal pain
- Depression or cognitive changes
-
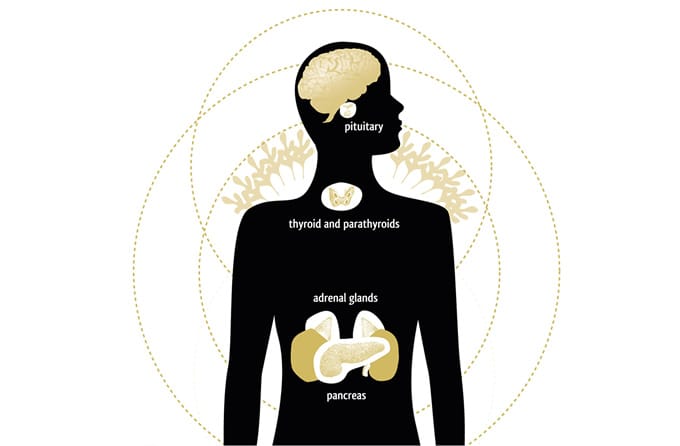 The Endocrine Glands
The Endocrine Glands
Pancreatic Neuroendocrine Tumors in MEN1
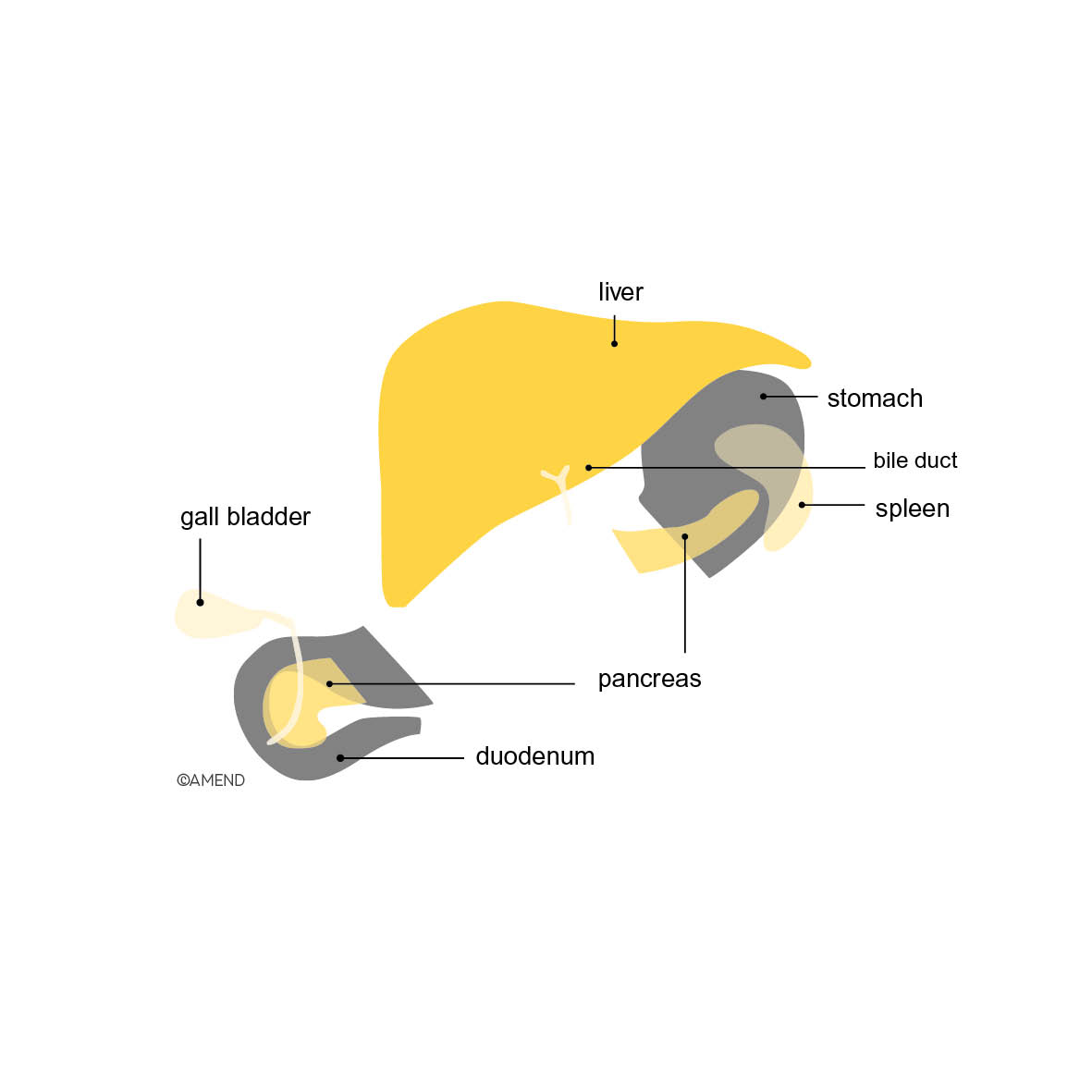
The pancreas lies in the abdomen behind the stomach and is connected to a part of the small intestines called the duodenum. It produces several hormones important for the body’s energy levels. 3 out of 4 (75%) of MEN1 patients will develop one of several pancreatic neuroendocrine tumors and 1 in 10 (10%) of those will develop more than one type of tumor. While the tumors may produce hormones, many are not active (non-functioning). Up to half of the tumors may become malignant (cancerous) if left untreated. Most pancreatic tumors are found using an MRI scan and blood tests. If the growths are very small, other types of scan may be used.
Treatment depends on the size and type of tumor. Anti-ulcer medications can be used to control symptoms of tumors called gastrinomas, but other types of tumor are usually treated with surgery. The operation may remove just the tumor, or remove the whole or a part of the pancreas. If the whole or a major part of the pancreas is removed, a patient will then have diabetes, which must be treated with regular insulin injections. Please note that the neuroendocrine pancreatic tumours of MEN1 are NOT the same as the more common pancreatic cancer, adenocarcinoma.
Those who develop pancreatic tumors may experience symptoms such as:
- Stomach ulcers (caused by gastrinomas, which increase stomach acid)
- Low blood sugar (caused by insulinomas, which produce excess insulin)
- Diarrhea or weight loss (caused by other hormone-secreting tumors)
- Flushing or rash (in rare cases, caused by tumors producing serotonin or other substances)
Pituitary Tumors in MEN1
The pituitary gland can be found at the base of the brain behind the nose, in a bony box called the sella turcica . It is very close to the optic nerves from the eyes and therefore, occasionally pituitary tumors can cause problems with vision. They may also cause headaches. 3 out of 10 (30%) of MEN1 patients will develop a pituitary tumor.
There are several different types of benign (non-cancerous) pituitary tumor, which can differ in size (microadenomas of less than 1cm in diameter, or macroadenomas of more than 1cm). All forms of pituitary tumor may be detected using an MRI or CT scan of the head as well as blood tests. Treatment may be in the form of medicine or surgery. This will depend upon the type of tumor and its size. Sometimes small tumors can be treated with tablets or injections although often surgery is needed.
The operation to remove a pituitary tumor is a relatively small one, and although carried out under general anesthetic, it does not involve having to operate on the main part of the head. Pituitary tumors are not brain tumours.
People with MEN1 who develop a pituitary tumor may experience:
- Headaches or vision problems (if the tumor presses on nearby structures)
- Irregular menstrual periods or infertility (due to prolactinomas)
- Growth abnormalities (in children, due to growth hormone imbalances)
- Fatigue, weight gain, or changes in skin and hair (due to adrenal imbalances or thyroid imbalances in cases of large tumors)
-
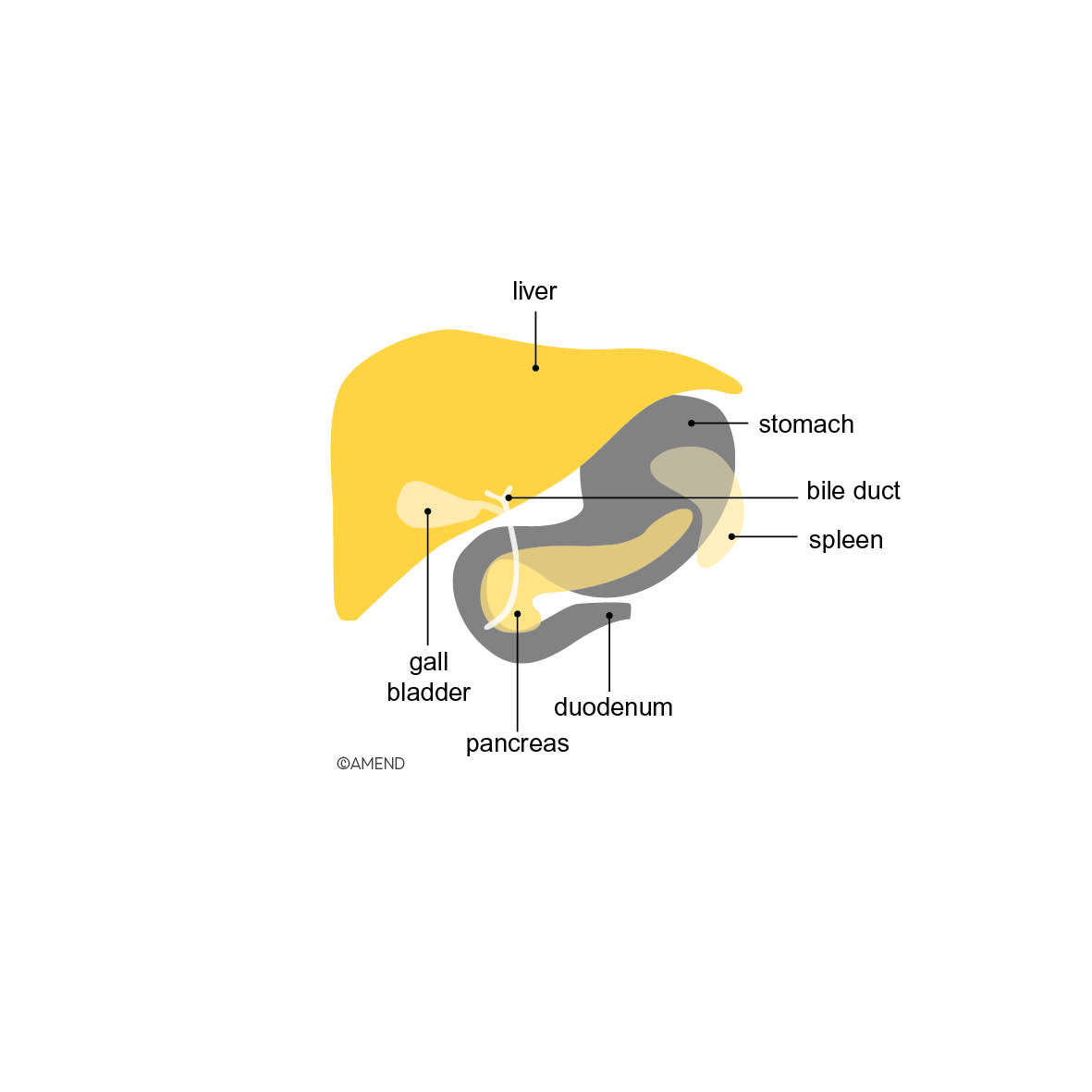 Location of the pancreas in the abdomen
Location of the pancreas in the abdomen -
 Whipple's Procedure diagram
Whipple's Procedure diagram
Who should be screened for MEN1?
Anyone with a family history of MEN1 or related tumors who also has one or more tumors in the parathyroid glands, pancreas, or pituitary gland should be screened for the syndrome. Alternatively, a family history of MEN1 with symptoms of hormonal imbalances, such as high calcium levels (hypercalcemia), stomach ulcers, low blood sugar, or unexplained changes in growth or menstrual cycles could be indicative of MEN1. Finally, a diagnosis of a rare endocrine tumor at a young age (e.g., before 30) may also be a sign of the disorder.
Additionally, MEN1 should be considered in individuals with a single MEN1-related tumor who have no family history but develop additional symptoms or tumors over time or have two of three of the trademarks of MEN1: hyperparathyroidism, pancreatic neuroendocrine tumors, or pituitary adenomas. Genetic testing can confirm a diagnosis of MEN1 in suspected cases.
What is the life expectancy of a person with MEN1 syndrome?
With early diagnosis, regular monitoring, and appropriate treatment, many people with MEN1 can live a normal or near-normal lifespan. However, complications from aggressive tumors or untreated hormonal imbalances can impact life expectancy. Advances in medical care and surgical techniques have significantly improved outcomes for MEN1 patients in recent years.
What is the age of onset for MEN1 syndrome?
MEN1 syndrome can manifest at different ages, but symptoms often appear in early adulthood. Parathyroid tumors, which are the most common type in MEN1, “onset in 90% of individuals is between ages 20 and 25 years with hypercalcemia evident by age 50 years” according to a publication in GeneReviews. However, cases have been reported in younger individuals, including teenagers and even children. The age of onset and the types of tumors can vary widely, even among members of the same family.
What cancers are associated with MEN1?
While most tumors in MEN1 are benign (non-cancerous), some can become cancerous over time. The most common cancers associated with MEN1 include:
- Pancreatic neuroendocrine tumors (pNETs), which can sometimes spread to other organs.
- Rarely, pituitary or parathyroid tumors may become cancerous.
- Carcinoid tumors, which can develop in the lungs, thymus, or gastrointestinal tract, are also a potential concern.
- Adrenocortical tumors may develop in the adrenal glands and are associated with hormone imbalances
How do you treat MEN1 syndrome?
Treatment for MEN1 syndrome focuses on managing the symptoms and complications caused by tumors. Common approaches include:
- Surgery: To remove tumors or affected glands, such as parathyroid glands or pancreatic tumors.
- Medications: To control hormone levels or symptoms, such as proton pump inhibitors for stomach ulcers caused by gastrinomas or dopamine agonists for prolactinomas.
- Regular monitoring: Blood tests and imaging scans (e.g., MRI or CT scans) are used to detect new tumors or changes in existing ones.
MEN1 is a genetic condition, and currently, there is no cure. However, with proper management, including regular screenings, timely surgeries, and medications, the symptoms and complications of MEN1 can often be controlled effectively. Research into genetic therapies and targeted treatments is ongoing, offering hope for improved management in the future.
Author: Jo Grey, AMEND CEO, with the help of the AMEND Medical Advisory Team. Updated by John Metzcar.
Further Reading
For further detailed information on MEN1, read AMEND USA’s MEN1 Patient Information Book (we recommend that you discuss the contents of this book with your specialist – it is not for use in self-diagnosis, and not all of the information it contains may be relevant to you).
-
MEN1 Patient Information Book

-
The Whipple's Procedure
Patient Stories
Click here to read patient stories about MEN1
-
My Story Template
Want to write your own story but don't know where to start? Use our handy template for inspiration! Scan and send by email or pop it in the post.
Click here to download